All about Cervical Cancer – Causes, Symptoms, Diagnosis, Treatment and Prevention

In India ,the overall cancer burden has more than doubled in the last three decades, the common ones being lung, mouth, breast, cervical and stomach. Many modifiable risk factors such as intake of highly
processed foods and sugary beverages, sedentary lifestyle, obesity, Type 2 diabetes, tobacco, alcohol consumption and environmental pollution contribute over and above the underlying genetic risk.
Cervical cancer is one of the most preventable as well as a very slowly growing cancer, yet in India, one in four women die of cervical cancer.
In this article, we will understand the Definition, Causes, Symptoms, Diagnosis, Treatment and Prevention of Cervical Cancer.
What is Cervical Cancer?
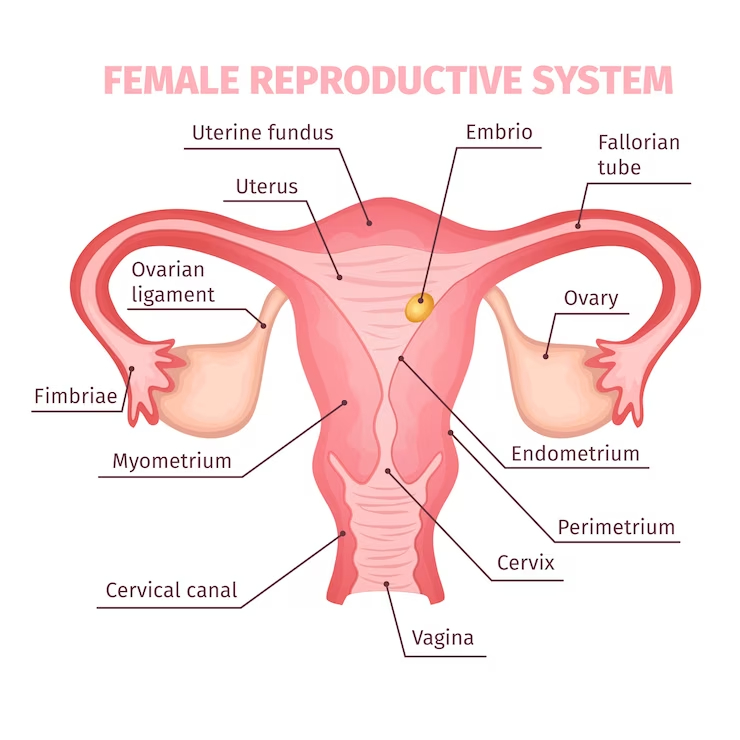
Cervical cancer is a cancer that starts in the cells of the cervix. The cervix is the neck of the uterus or womb and connects the uterus to vagina (see reference picture below). It is normally quite tightly shut, with only a small opening that allows the menstrual blood flow out during a period and lets sperms in at time of intercourse.
During a normal delivery, the cervix opens up completely to let the baby out.
Causes
Long lasting HPV infection causes almost all cervical cancers.
There are over 100 subtypes of HPV viruses of which about a dozen are cancer causing or oncogenic. Most women will clear the HPV infections from their bodies (85% in 1 year and 98% in 2 years) and very few will have persistent infection that can progress to pre-cancer and cancer, and this gives a window of opportunity to diagnose it early.
Multiple sexual partners increase the risk of HPV infections and condom use reduces the same.
Symptoms
- Pre-cancerous cell changes do not usually have any symptoms.
- Bleeding from the vagina at other times than when one is having a period (i.e. between periods, after or during sex, any time after menopause) is the commonest symptom.
- Some women may have a vaginal discharge that smells unpleasant or is blood stained or discomfort or pain during sex.
Methods of Diagnosis
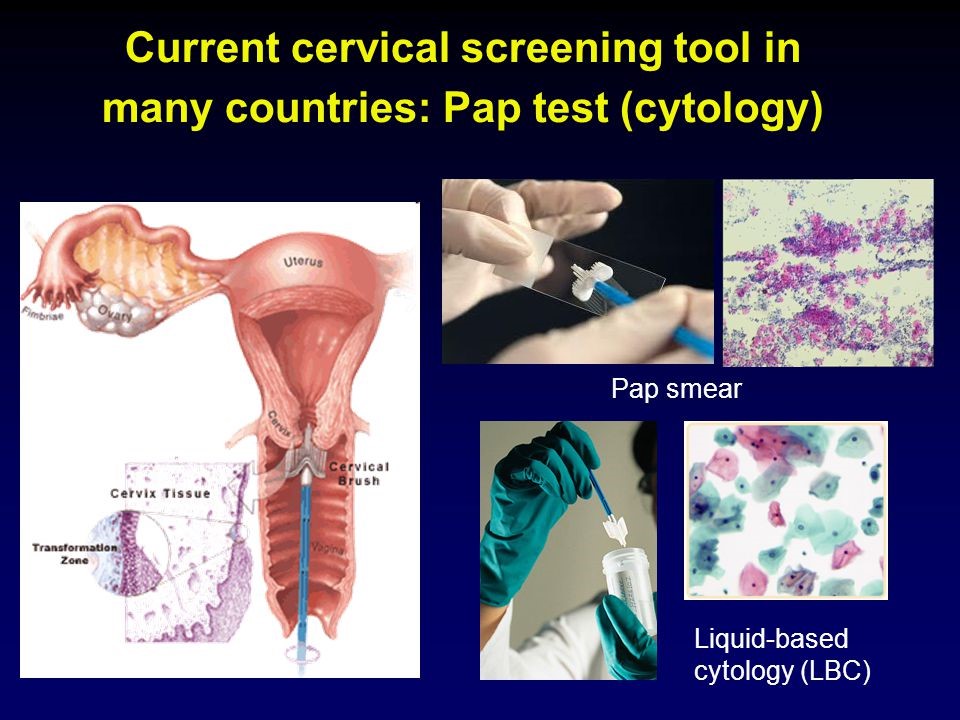
Screening tests are done in all women (asymptomatic) to estimate risk of development of cancer.
For cervical cancer, these are hr HPV (high risk HPV test), LBC (liquid based cytology), Pap Smear, VIA and VILI (visual inspection with acetic acid and visual inspection with Lugol’s iodine).
Of the above, first two are most sensitive but expensive compared to the pap smear but VIA and VILI can be done most easily with training of even nursing personnel to screen women even in rural areas without much infrastructure.
If a woman does one of these tests even once in a lifetime, it can reduce the number of women dying from cervical cancer by 50%.
Self sampling HPV kits are being developed indigenously and will soon be available and affordable.
Recommended screening interval is every 3 years for Pap smear & VIA/VILI, and every 5 years for combined hr HPV and LBC starting within 3 years of being sexually active till the age of 65 years.
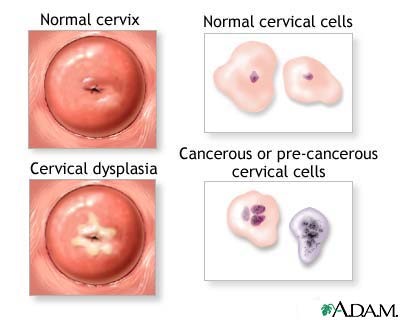
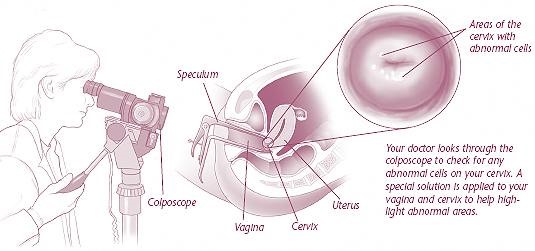
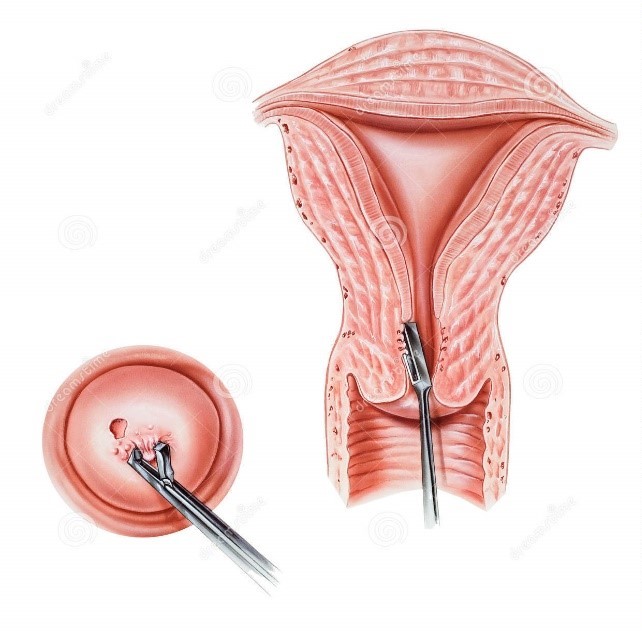
Confirmation of the diagnosis of cervical cancer or pre-cancer requires a biopsy of the cervix. This is
often done through colposcopy – a magnified visual inspection of the cervix aided by using an acetic acid solution to highlight abnormal cells on the surface of the cervix.
Modalities of Treatment
All the treatments aim to do the same thing – remove or destroy the abnormal cells.
- In precancerous stages, Laser ablation, cold coagulation, and cryotherapy can treat just the part of the cervix that contains abnormal cells. This allows normal cells to grow back in their place. Thus the cervix remains functional without effect on childbirth.
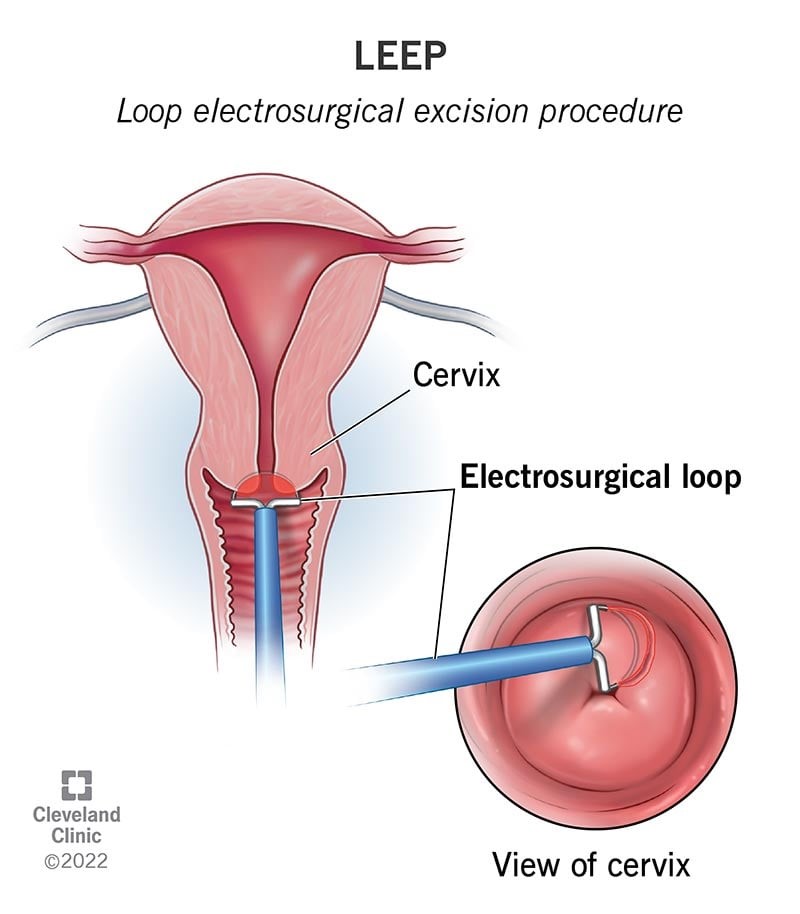
- LEEP and cone biopsy remove the whole area of the transformation zone – the area containing all the cells that could develop into cervical cancer and can weaken the cervix and increase risk of abortions.
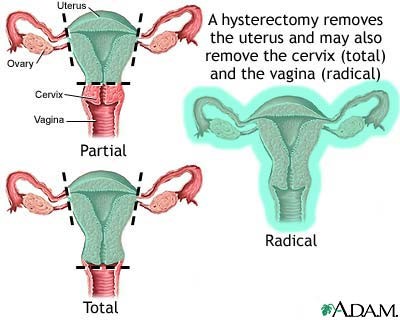
- Hysterectomy is offered to women who have completed child-bearing. This may be total or radical depending on the stage of cancer.
- Certain cervical cancers also respond well to Radiotherapy so depending on the stage and type of cancer, patient may require only Surgery or only Radiotherapy, or both, or a combination of Surgery, Radiotherapy and Chemotherapy.
When cervical cancer is diagnosed at an early stage, the 5 year relative survival rate is 92% but if diagnosed when it has spread to nearby tissues, organs or regional lymph nodes, it is 59%
Investigations and regular follow-up is advisable after the treatment.
Prevention by Vaccination
Globally, cervical cancer incidents continue to decline thanks to established screening programmes and widespread uptake of HPV vaccine by adolescent girls. In India too, cervical cancer has reduced by 39.4% but we can do much better as one in five cases of cervical cancer is in India.
- HPV vaccine is recommended for routine vaccination for girls and boys at 11-12 years (Can be started at age 9). Catch up vaccination from 13 -26 years can be given if not vaccinated when younger.
- HPV vaccination is given in a series of either two or three doses depending on age at initial vaccination.
- Some adults from 27-45 years may decide to get the vaccination after discussion with the health provider as it provides less benefit as they may have been already exposed to the virus (after being sexually active) and this includes post partum vaccination (after childbirth).
- Vaccine is contraindicated during pregnancy.
- Screening tests should be done in vaccinated women albeit at longer intervals.
Robust vaccination programmes in some countries have reduced the incidence of cervical cancer by 90%. Current HPV vaccines protect mainly against 16 & 18 (responsible for 70% of cervical cancers), and are being updated to cover more oncogenic subtypes.
Indian government is in process of launching an indigenous low cost cervical cancer vaccine. It aims to cover 90% of girls under 15 years with vaccine, 70% of women with screening to reduce cervical cancer mortality by 30%.
We at the GSBS Medical Trust offer regular cervical cancer screening with Pap smear testing. Do avail of the facility and spread the awareness regarding cervical cancer.

By Dr. Deepali Prabhat
MD, DGO, DFP, FCPS, DNB, MPS, Dip IBLM -- Consultant Obstetrician, Gynaecologist and Life Style Medicine Specialist